
Attention deficit hyperactivity disorder (ADHD) and Attention Deficit Disorder (ADD now sometimes called Inattentive ADHD) are conditions that can occur in a percentage of children. Symptoms of ADHD include trouble concentrating, paying attention, staying organized, and remembering details.
It can be a difficult condition to diagnose as there are no medical tests such as blood tests that can give a categorical answer. Diagnosis can rely on perceptions of behaviour from school teachers, parents and health professionals. Children with untreated ADHD are sometimes mis-labelled as troublemakers or problem children.
Find out more about ADHD from NHS.UK by clicking here.
However, there are some reasons why children might have some symptoms that overlap with ADHD symptoms but care caused by sleeping problems. Symptoms similar to those of ADHD may be caused by:
There are some potentially simple treatments available for children that do not have ADHD but are presenting with similar symptoms. If appropriate, these daily routine changes can help some children, with sleeping problems to redude these syptoms.
It could therefore helpful to rule these alternative causes before a diagnosis of ADHD is confirmed and before any medication is considered.
Here is more detail on some of the conditions that may produce ADHD-like symptoms

The symptoms of sleep deprivation in children resemble those of ADHD. While adults experience sleep deprivation as drowsiness and sluggishness, sleepy children can become more wired and moody. They may have trouble focusing, sitting still and getting along with peers. Sleep research has reported that chronic poor sleep results in daytime tiredness, difficulties with focused attention, irritability and frustration, and impulsivity (1).
Similarly, the quantity of sleep in 7-12 year old children was found to be significantly associated with behavioural symptoms including aggressive and disruptive behaviour. (2)
Sleep deprivation makes it difficult to learn and impairs mood. More surprisingly, partial, or low-level, sleep deprivation has a bigger effect on behaviour than either short or long-term complete sleep deprivation.
This means that some children may be mis-diagnosed with ADHD/ADD when the real problem is chronic or partial sleep deprivation.
There are other reasons as well that may lead to children being misdiagnosed with ADHD/ ADD, including snoring/ sleep apnea.
Snoring is a possible symptom of a condition called Sleep Apnea. The peak age is 2-5 – coincidentally the same age ADHD is often considered. (If your child snores they don’t definitely have Sleep Apnea though. Take a recording on your smart-phone and go to see your GP for advice.)
Classically, those with sleep apnea snore quite loudly for a bit, then are silent, maybe pause in breathing, then snort briefly, move about, and resume snoring.
Children with sleep apnea do not get sound sleep. They may also get less oxygen to the brain at night. Obstructive sleep apnea can have a serious negative impact on a child’s intellect and behaviour. The common symptoms of sleep apnea are difficulty paying attention during the day, decreased academic performance, oppositional behaviour, and restlessness – the same symptoms as ADHD.
Another study suggesting a link between snoring, sleep apnea and ADHD symptoms followed 11,000 British children for six years, starting when they were 6 months old. The children whose sleep was affected by breathing problems like snoring, mouth breathing or apnea were 40 percent to 100 percent more likely than normal breathers to develop behavioural problems resembling ADHD (Paediatrics March, 2012)
“Lack of sleep is an insult to a child’s developing body and mind that can have a huge impact,” said Dr Karen Bonuck, the study’s lead author. “It’s incredible that we don’t screen for sleep problems the way we screen for vision and hearing problems.”
Large adenoids and tonsils can cause sleep apnea and removing the adenoids and tonsils can clear the symptoms very quickly.
Research shows that children with nighttime breathing problems did better with cognitive and attention-directed tasks and had fewer behavioural issues after their adenoids and tonsils were removed. The children were significantly less likely than untreated children with sleep-disordered breathing to be given an ADHD. diagnosis in the ensuing months and years.
“We’re getting closer and closer to a causal claim” between breathing problems during sleep and ADHD symptoms in some children, said Dr. Ronald Chervin, a neurologist and director of University of Michigan Sleep Disorders Center in Ann Arbor.

A child eating too much sugar and some food additives may have their sleep affected. Sugar and some food additives can also directly impact on behaviour – parents are usually familiar with ‘sugar rushes’ and food additives have a similar effect. It’s best to limit sugar – certainly avoid sugar near bed time – and to cut out food additives altogether if you suspect they effect your child. Click here to read more information on ‘Food Colours and Hyperactivity’ from the NHS.
Children with sleepwalking, restless leg syndrome, narcolepsy, insomnia, or other sleep problems may also be misdiagnosed with ADHD or ADD. All of these issues may need to be referred to a paediatrician or specialist sleep clinic to assess your child and recommend treatment. Restless Leg Syndrome is often managed well with a magnesium supplement. Talk to your GP about this.
Magnesium and iron are both necessary elements. Good sources of magnesium include almonds, other nuts and green leafy vegetables. The most common symptoms of magnesium deficiency are tics, muscle spasms, restless leg syndrome, and anxiety – and sleeplessness and stress result in magnesium being further flushed out of the body.
Magnesium has been called “nature’s muscle relaxant.” It calms the central nervous system and can act as a sedative. Magnesium actually suppresses nerve activity, which leads to a decrease in muscle twitches and jerks, therefore decreasing incidents of night waking. For these reasons, healthy levels of magnesium have been linked to deep, undisturbed sleep.
Melatonin is sometimes prescribed for children with diagnosed sleep problems in the UK.
Summer-born children – those born in June, July and August in England and Wales – were 1.3 times more likely than the oldest quarter of children in the school year to be diagnosed with intellectual disability, 1.4 times more likely to be diagnosed with attention deficit hyperactivity disorder, and 1.3 times more likely to be diagnosed with depression.
The paper, published in JAMA Pediatrics in 2019, pointed out that younger children may find it harder to concentrate, leading to overdiagnosis of hyperactivity. Other issues such as lower academic performance and poorer peer relationships can also lead to mental health problems.
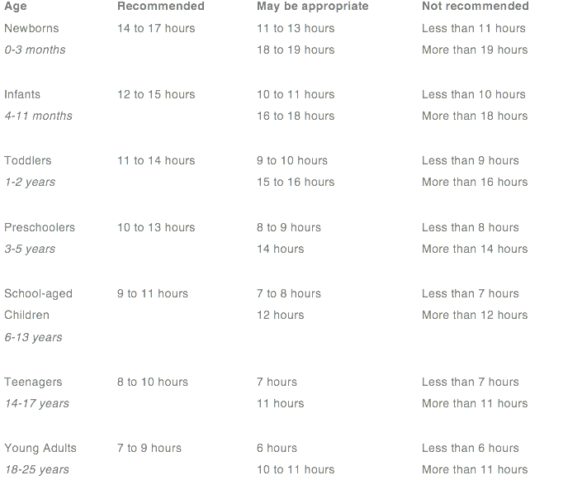
This table shows the amount of sleep recommended for each age group.
Source – US National Sleep Institute.
If your child is displaying symptoms of ADHD such as trouble concentrating, paying attention, staying organized, and remembering details, ask the following questions before considering a diagnosis of ADHD.
1) Is my child sleeping long enough? Refer to the Table.
2) Does my child snore?
3) Does my child’s legs twitch when they sleep – sometimes even waking them up?
4) Does my child have any other sleep disorders, including night terrors or sleep walking?
5) Is your child young for their class?
6) Are you or your child’s teacher comparing your child’s behaviour to other children in their class – or to other children the same age?
7) Does your child have a good sleep routine?
8) Do they go to sleep easily and sleep through the night?
9) Do they often wake up early in the morning? At the same time?
10) Does your child eat a healthy diet?
11) Does your child eat a lot of processed food, E numbers and/ or sugar?
Once you’ve ruled out all the questions above at home, and if the symptoms are still evident, speak to your GP.
If you are still concerned that your child may have ADHD
If you have looked at your child’s sleep and other aspects of their routine and their symptoms haven’t improved you can speak to your child’s GP about ADHD to seek a diagnosis. Here is some further information about the diagnosis and treatment of ADHD from the NHS as medication can really help some children with a diagnosis of ADHD:
https://www.nhs.uk/conditions/attention-deficit-hyperactivity-disorder-adhd/
Adams, SK, and TS Kisler. “Sleep quality as a mediator between technology-related sleep quality, depression and anxiety.” Cyberpsychol Behav Soc Netw. 2013; 16(1): 25-30.
Aronen, A et al. “Sleep and Psychiatric Symptoms in School-Age Children.” Journal of the American Academy of Child and Adolescent Psychiatry. April 2000, 39(4): 502-508.
Centers for Disease Control and Prevention (CDC). “Increasing prevalence of parent-reported attention-deficit/ hyperactivity disorder among children – United States, 2003-2007.” Morbidity and Mortality Weekly Report, 2010; 59 (44): 1439-43.
Cooper, WO et al. “ADHD drugs and serious cardiovascular events in children and young adults.” N Engl J Med. 2011; 365(20): 1896-904.
Elder, TE. “The importance of relative standards in ADHD diagnoses: evidence based on exact birth dates.” J Health Econ. 2010; 29(5): 641-56.
Hale, L, and S Guan. “Screen time and sleep among school-aged children and adolescents: a systematic literature review.” Sleep Med Rev. 2015; 21: 50-18.
Mayes, R et al. “ADHD and the rise in stimulant use among children.” Harv Rev Psychiatry. 2008; 16(3): 151-66.
Mosholder, AD et al. “Hallucinations and other psychotic symptoms associated with the use of attention-deficit/ hyperactivity disorder drugs in children.” Paediatrics. 2009; 123(2): 611-16.
National Institute for Clinical Excellence. “Attention Deficit Hyperactivity Disorder: Diagnosis and Management of ADHD in Children, Young People and Adults.” NICE Clinical Guidelines. 2008: 72:6.
Seminars in Pediatric Neurology, Mar 1996. Vol 3, Issue 1, p 1 – 50. Sleep Disorders in Childhood.
Sleator, EK, and RK Ullmann. “Can the physician diagnose hyperactivity in the office?” Pediatrics. 1981; 67(1):13-17.
Swanson, JM et al. “Effects of stimulant medication on growth rates across 3 years in the MTA follow up.” J Am Acad Child Adolesc Psychiatry. 2007; 46(8): 1015-27.